At my lab we use Elecsys HIV Duo for HIV screening. The HIV Duo is a fourth-generation HIV test meaning that it detects both p24 antigen (Ag) and antibodies (Ab) to HIV, shortening the time of detection to 2-3 weeks after infection.
The HIV Duo is an Electrochemiluminiscence Immuno Assay (ECLIA):
For HIV p24 Ag detection, two types of monoclonal antibodies are mixed with the blood sample. The first type of antibodies are labeled with biotin and the second type with Ruthenium. These bind to p24 Ag in the patient sample and form a sandwich complex.
Similarly , for HIV Ab detection, two types of HIV specific recombinant antigens/peptides are mixed with the blood sample. The first type of antigen is labeled with biotin and the second type with Ruthenium. These bind to HIV Ab in the patient sample and form a sandwich complex.
Micro-beads coated with Streptavidin are added to the mix. The biotin in sandwich complex binds to Streptavidin and the micro-beads are magnetically attached to a measuring cell.
When voltage is applied, Ruthenium emits light that can be detected by a photo multiplier.
HIV Ag and Ab can be detected in parallel and depending on the result we use different confirmatory assays to confirm the results, but that is outside of the scope of this review.
How good are our screening tests?
According to Roche, the maker of Elecsys HIV Duo, the sensitivity of the HIV Duo is 100% and the specificity somewhere in the range of 99.87-99.92% depending on what study you look at.
My point here is that this can vary widely depending on the population you’re testing and I will exemplify that by a study from Tanzania.
Everett et al. sought out to determine the specificity of the Abbott Murex HIV antigen/antibody combination enzyme immunoassay (EIA) for the diagnosis of HIV infection in Tanzania. The Abbot Murex is another fourth-generation HIV test with a stated sensitivity of 99% and specificity of 99%.
When testing 7333 Tanzanian adolescents and young adults (age 16–27 years) they found a much higher rate of false positives than expected and calculated the specificity of the test in this setting to 91.5%.
What causes false positive results?
To investigate the factors associated with the high rate of false-positive test results observed, Everett et al. conducted another study on the same cohort and found that false positivity was strongly associated with increasing levels of Schistosoma haematobium worm IgG1 antibodies.
Similar findings can be observed with in other infections. For example, Gudipati et al. examined 31 910 medical records on patients PCR tested for SARS-CoV-2 within 2 weeks of an HIV fourth-generation assay. They found that patients with positive SARS-CoV-2 PCR tests were significantly more likely to have a false positive fourth-generation HIV test than those with negative SARS-CoV-2 PCR tests.

Similar findings can also be observed in non-infectious diseases. For example, Chiu et al. conducted a retrospective study of cancer patients. The patients were seen at the University of Texas MD Anderson Cancer Center and had a variety of types of cancer. Of 43 637 patients that underwent HIV screening, 272 cancer patients were positive. Of these as many as 29% (n=78) of the positive results were false positive.
What causes the false positive reaction?
In a review article in Expert Review of Anti-infective Therapy the authors note that:
Heightened CD5+ B-lymphocyte activation in the early immune response to infectious disease antigens produces broad-spectrum antibodies that can cause nonspecific and unpredictable cross-reactivity in serological testing.
They propose that early B-lymphocyte response/polyspecific cross-reactivity can be a significant cause of HIV false-positive results, with the implication that test characteristics may vary significantly in different geographical areas and among different populations.
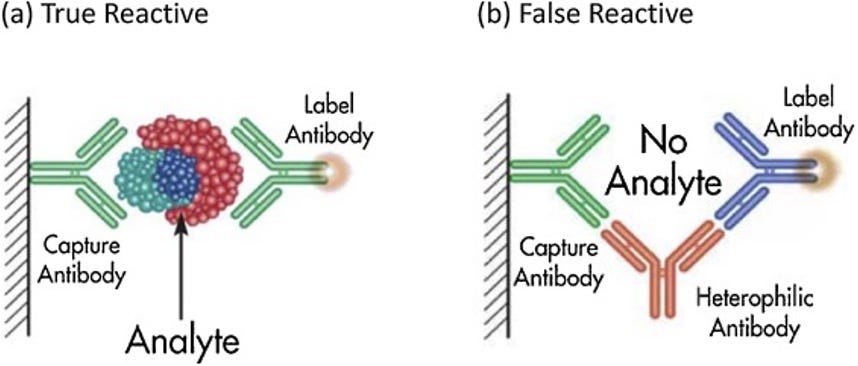
This means that the false positive reactions can be unpredictable. We recently had a case at our lab were a false positive HIV test, after thorough testing, were attributed to a concurrent infection with Epstein-Barr Virus (EBV). This does not mean that EBV necessarily is similar in antigen structure to HIV. EBV infection induces specific antibodies to EBV and various unrelated non-EBV heterophile antibodies. These heterophile antibodies are generally weak antibodies with multi-specific activities which can create sandwich complex without the presence of the analyte you’re looking for.



Elecsys duo on e801 or other system?